This guideline has now been superseeded by the 2015 intubation guidelines click here
Rapid sequence induction, non-pregnant adult patient, no predicted difficulty
Each step of the guideline is described.
This case scenario is of an adult, non-pregnant patient undergoing a rapid sequence induction. This is a common anaesthetic technique in the UK when there is a risk of gastro-oesophageal reflux.
The anaesthetic technique includes optimal preoxygenation, the use of an induction agent and suxamethonium, with the application of 30 N cricoid force at the onset of unconsciousness.
Preoperative airway evaluation has not predicted any problem with airway management. Airway evaluation is imperfect and so airway strategy must deal with unexpected difficult direct laryngoscopy and difficult facemask ventilation.
In this case scenario, the urgency of the surgery is not immediate and failure of intubation activates a plan of 'wake-up'
The scenario of a rapid sequence induction when surgery is immediately urgent (for example in extremis aortic aneurysm rupture) is not considered here in detail. (Please note that the quality of guideline image is low to aid fast loading. The pdf file download is good quality.)
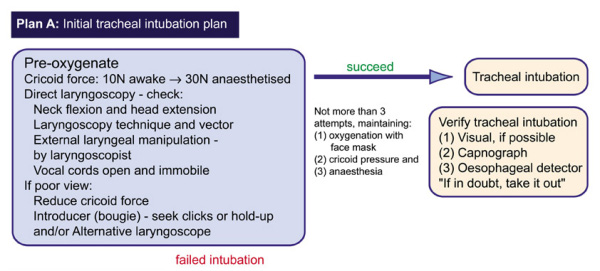
PLAN A
 Notes:
-
Notes:
-
- Standard set-up for RSI.
- Adjust head/neck position prior to starting.
- Optimal preoxygenation.
- Induction agent and suxamethonium.
- Cricoid cartilage identified before induction by assistant.
- Light pressure (no more than 10 N force) on the cricoid cartilage prior to loss of consciousness.
- 30 N cricoid force (equivalent to registering 3 kg on a weighing machine) after loss of consciousness.
- Direct laryngsocopy undertaken.
- If difficult try alternative blade (long, straight, McCoy etc), bougie, and the limited amount of external laryngeal manipulation possible with cricoid force.
- If intubation unsuccessful - stop further attempts. Do not give second dose of relaxant.
- Announce 'Failed intubation' to stop yourself carrying on with further attempts and to alert assistant that Plan A has failed.
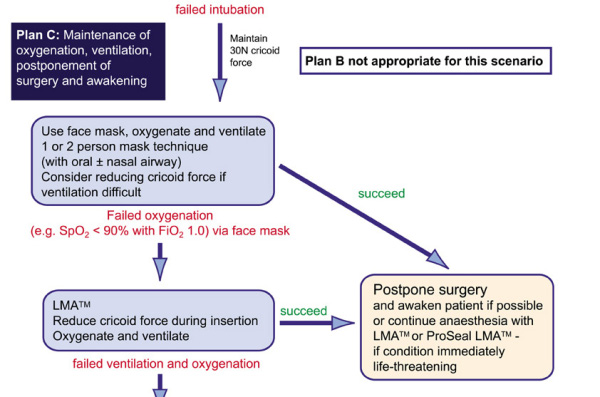
PLAN B
Notes: There is no intubation Plan B because the patient is going to be woken up without any other attempts at intubation. The only task now is to move to Plan C - the maintenance of oxygenation whilst the induction agent and muscle relaxation wear off and the patient awakens.
PLAN C
 Notes:
Notes:
- Call for assistance and keep first responder.
- Continue cricoid force at 30 N.
- Insert oral airway and attempt facemask ventilation with 100% oxygen.
- If necessary use two hands to hold facemask and ask responder to squeeze bag.
- If facemask inflation not possible, maintain 30 N cricoid force and insert laryngeal mask. Release cricoid force as laryngeal mask is inserted and reapply when inserted.
- Attempt to ventilate with 100% oxygen via laryngeal mask with cricoid force.
- If that fails release cricoid force and try ventilation again through the laryngeal mask.
- If ventilation is still not possible, and the patient is not awakening/struggling to breathe and the saturations have fallen below 85% go on to Plan D (failed intubation and failed ventilation).
PLAN D
 Notes:
This is considered in another flow-chart.
Notes:
This is considered in another flow-chart.
Areas for Discussion in 2006
- Gentle facemask ventilation (inspiratory pressure less than 20 cm water) is acceptable to some experienced practitioners during the period of waiting for the relaxant to work. Is this reasonable?
- Whilst it is good practice to identify the cricoid cartilage before induction, should any force be applied before loss of consciousness?
- The flow-chart is not relevant for the use of a non-depolarizing relaxant instead of suxamethonium. Is there a role for the Proseal in this circumstance (if so it should be in theatre at the start of induction)?
- If the operation must proceed even if intubation fails, what are the relative merits of muscle relaxation vs letting the patient breathe (or possibly struggle)?
- If the surgery must proceed (or a long acting relaxant is given) what are the relative merits of using the Proseal vs trying to intubate via the ILMA.? Does the prior presence of a nasogastric tube influence the decision?
